Introduction
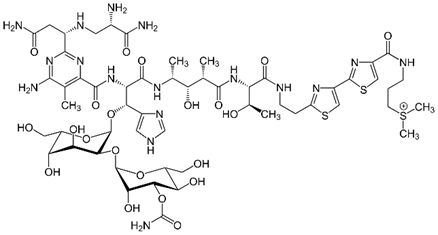
Breast cancer is a malignant neoplasm that develops from the glandular cells of the breast and can grow invasively in the breast and metastasise to distant organs such as the lungs, liver or bones. It is the most commonly diagnosed malignant tumour in women, but it is worth noting that it can also occur in men.
Although the exact causes of breast cancer are not fully understood, there are some factors that increase the risk of developing the disease:
- Age: The risk increases with age, especially after the age of 50.
- Family history: If there is a family history of breast cancer, the risk of developing the disease increases.
- Genetic mutations: Mutations in the BRCA1 and BRCA2 genes significantly increase the risk of breast cancer.
- Obesity and physical inactivity: Overweight and obesity are associated with an increased risk.
- Early menstruation and late menopause: Early onset of menstruation and late menopause may increase risk.
- Hormone replacement therapy: Long-term use of hormone replacement therapy may increase risk.
- Lack of breastfeeding: Women who have never breastfed may have a slightly higher risk.
It is important to remember that having one or more risk factors does not mean that you will definitely get breast cancer. Many women with risk factors will never get the disease.
Regular preventive examinations, such as mammography and breast self-examination, are the best way to detect breast cancer early and increase the chances of successful treatment.
Cancer patients can be divided into two main groups:
- Patients with the possibility of a cure: These are patients in whom the disease has been detected at an early stage or at localised stage (stage I-III). The aim of treatment is the complete removal of the tumour.
- Patients with palliative treatment: These are patients with metastases to distant organs (stage IV), in whom treatment aims primarily to improve quality of life by alleviating the symptoms of the disease and prolonging survival. The possibility of a complete cure in these cases is limited.
Diagnosis and treatment
As we are chemists, we would like to introduce you to modern treatment methods from a chemical point of view. We will try to describe them in an accessible way. However, before treatment can begin, a diagnosis is needed.
Diagnosis is based primarily on mammography and breast ultrasound.
Mammography and breast ultrasound are the primary imaging examinations in the diagnosis of breast cancer.
They are used for:
- Early detection of breast lesions: They often allow cancerous changes to be detected long before clinical symptoms such as pain or a palpable lump appear.
- Assessing the size and nature of lesions: Based on these examinations, the doctor can determine the size of the lesion, its position in the breast and assess whether it has cancerous features.
- Conducting further diagnostics: If the results of mammography or ultrasound are inconclusive or indicate the presence of suspicious lesions, a thick-needle biopsy may be necessary. This test involves taking a small amount of tissue from the nodule for thorough histopathological examination.
Why is axillary fossa assessment so important?
- Spread of the cancer: Breast cancer can spread to lymph nodes located in the axillary pits.
- Treatment planning: Information about lymph node involvement is crucial when deciding on treatment.
When are these tests performed?
- Regular preventive examinations: Women should have regular mammography and breast ultrasound as recommended by their doctor.
- In case of symptoms: If a woman notices any changes in her breasts, such as a lump, thickening of the skin, retraction of the nipple, she should see her doctor.
Is this all?
In addition to mammography and ultrasound, in some cases additional tests may be necessary, such as:
- Magnetic Resonance Imaging (MRI): Particularly useful in cases of dense breast tissue, when mammography is less effective.
- Computed tomography (CT): Used to assess metastases to other organs.
- Pet-CT: Combination of CT and positron emission tomography for accurate assessment of the extent of disease.
However, the basics are also based on self-prevention and breast self-examination once a month. You are encouraged to read about how to perform the self-examination correctly here: https://pacjent.gov.pl/aktualnosc/jak-prawidlowo-wykonac-samobadanie-piersi
Breast cancer treatment is individual - it depends on many factors, such as the stage of the disease, the type of cancer, the patient's age and her general health. Usually several treatment methods are combined to achieve the best possible results.
Primary treatments for breast cancer:
- Surgery:
- Lumpectomy: Removal of the tumour along with a small margin of healthy tissue.
- Mastectomy: Removal of the entire breast.
- Lymph node excision: Removal of lymph nodes to check if the cancer has spread.
- Radiotherapy: The use of ionising radiation to destroy cancer cells. Often used after breast-sparing surgery.
- Chemotherapy: The use of anti-cancer drugs that reach throughout the body and destroy cancer cells.
- Hormone therapy: Used for hormone-dependent cancers. The drugs block the action of hormones that stimulate the growth of cancer cells.
- Targeted therapy: Drugs act on specific features of cancer cells to minimise damage to healthy tissues.
- Immunotherapy: Stimulates the patient's immune system to fight cancer cells.
Chemotherapy is one of the primary treatments for systemic breast cancer. It involves the administration of anti-cancer drugs, called cytostatics, which are designed to destroy cancer cells. Unfortunately, these drugs are unable to distinguish between cancer cells and healthy cells and often damage healthy tissue as well, leading to a number of unwanted side effects.
When is chemotherapy used?
Chemotherapy is used both to treat the early stages of breast cancer, before or after surgery, and in advanced stages of the disease when the cancer has spread to other parts of the body.
How does chemotherapy work?
Chemotherapy drugs are usually administered to the body intravenously. They enter the bloodstream and spread throughout the body, reaching all areas where cancer cells may be present. These drugs act on rapidly dividing cells, both cancerous and healthy. Unfortunately, cancer cells divide much faster than healthy cells and are therefore more sensitive to the effects of chemotherapy.
Side effects of chemotherapy
Unfortunately, chemotherapy is associated with a number of side effects, which can include:
- Hair loss
- Nausea and vomiting
- Reduction in blood cell count
- Skin changes
- Changes in taste and appetite
- Fatigue
- Other: Other side effects may also occur, such as neurological disorders, heart problems, kidney damage.
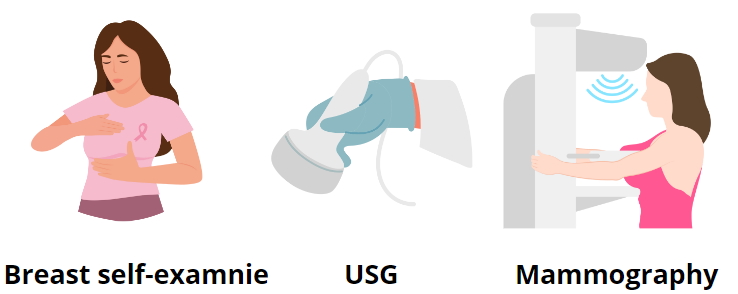
Compounds used in chemotherapy
Despite the long introduction, which we feel was much needed to illustrate what we are dealing with, it was time to get down to what chemists know best - chemistry. Most of us surely associate the orange drips from the movies. In fact, there are 3 chemistries in the treatment of breast cancer: red, yellow and white. Let's take a look at what we can find in them.
The so-called ‘red chemo’ is a colloquial term for any chemotherapy that includes drugs from the anthracycline group: doxorubicin or epirubicin.
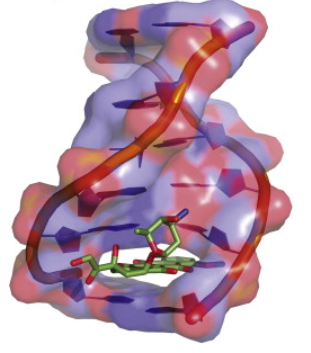
I will focus here on doxorubicin. Doxorubicin is a potent anticancer drug that acts through several mechanisms, damaging cancer cells and inhibiting their growth. Doxorubicin binds to the DNA of cancer cells, causing damage to their structure. The flat aromatic chromophore part of the molecule inserts between two DNA base pairs, while the six-membered sugar is located in a smaller groove and interacts with adjacent base pairs immediately adjacent to the insertion site, as evidenced by numerous crystal structures. This prevents cells from dividing properly and leads to cell death.
Yellow chemotherapy is mainly used as complementary treatment in breast cancer. It mainly consists of 3 drugs: methotrexate, cyclophosphamide and 5-fluorouracil. It is methotrexate that is responsible for the yellow colour of the solution. Methotrexate is a powerful anti-cancer drug that works by interfering with the processes necessary for the growth and multiplication of cancer cells. Its main mechanisms of action are Blocking DNA synthesis. Methotrexate inhibits the enzyme dihydrofolate reductase, which is essential for the production of folic acid. Folic acid, in turn, is essential for DNA synthesis. By blocking this enzyme, methotrexate prevents cancer cells from forming new DNA, which inhibits their division and leads to death.
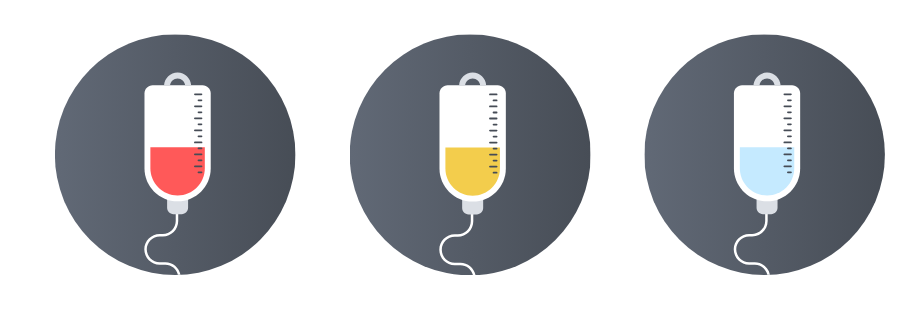
The white chemo in its formulation has mainly bleomycin. Bleomycin is an anticancer drug that works on a slightly different principle than many other chemotherapeutics. Its main mechanism of action is direct damage to the DNA of cancer cells. Bleomycin binds to the DNA of the cancer cell and causes it to break. This prevents the cell from functioning properly and leads to its death. It is also speculated that bleomycin contributes to the formation of highly reactive molecules, so-called free radicals, in cancer cells. These molecules damage various components of the cell, accelerating its death.
A precious metal to the rescue!
We are talking here about the complex compounds PLATIN. Specifically cisplatin, carboplatin and oxaliplatin. Although only cisplatin is used for specific types of breast cancer on an ad hoc basis, the next two are already used for severe cases such as malignant tumours of the reproductive organs or even sarcomas.
We hope that we have at least given you some idea of the problem of breast cancer and the available methods of treating it. Remember that not every tumour is immediately cancerous, but until there is biopsy confirmation, every case is considered malignant.
Get tested and remember that there are superheroes like red, white, yellow chemo, hormone therapy or immunotherapy, and for the most stubborn there is platinum.
HEALTH !!!
Where did we get our knowledge from? From these sites worth looking at:
https://www.zwrotnikraka.pl/
https://onkologia.org.pl/pl
https://www.amazonkifederacja.pl/
https://alivia.org.pl/
https://centrumkryzysowe.org.pl/
Text: Agnieszka Kicińska
Editors: Agnieszka Kicińska, Maciej Gdala, Kinga Adamiec
Graphic design: Agnieszka Kicińska, internet sources